For more than 20 years, IPMS has been a leading provider in revenue cycle management services to medical practices. Our success is built on fostering solid relationships with our clients and delivering superior business support that drives revenue growth and creates real, tangible outcomes.
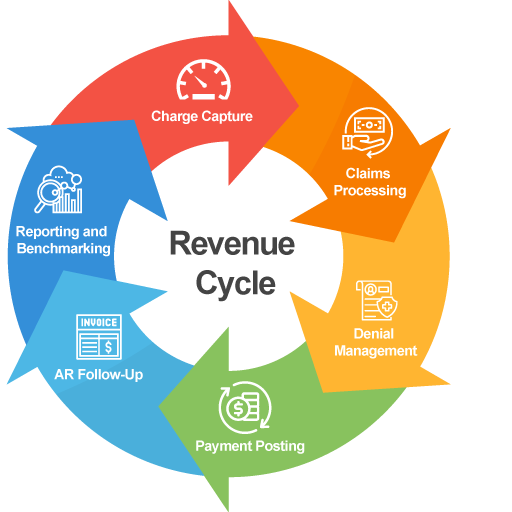
Our rigorous approach to revenue cycle management, strict adherence to deadlines, frequent communication and timely follow-ups deliver results well-above MGMA benchmarks. We leverage our team of industry veterans to ensure every aspect of the revenue cycle is processed in the most efficient and effective manner possible.
We start by pairing you with a dedicated Account Manager, an experienced industry veteran and your point of contact. Our Account Managers will assure that every service rendered is accounted for and fully paid. They work to incorporate your practice’s unique processes and regularly evaluate performance for continued success.
- Maximize reimbursements through a combination of strategic processes and services
- Reduce operational costs and enhance efficiencies
- Ensure the rapid processing of claims submissions, payments, denials, and correspondence
- Deliver the support of industry veterans who carry out what we promise and stay ahead of an ever-changing industry
- Provide frequent communication and outstanding customer service
- Provide comprehensive reporting with the option of customized reports
- Maintain secure electronic storage of patient data
Payer credentialing is a critical process to ensure payments are received in full for the medical services you provide. However, it is often a complex, resource-intense, and time-consuming task to accomplish. Our expert staff can complete all the necessary paperwork so your practice can focus on providing care for your patients.
- Prevent lost income incurred from late or missed renewals
- Improve your credentialing process in meaningful ways
- Build vital connections with insurance companies and serve more patients
- Become credentialed faster and safer
- Obtain, track, and submit all applications on your behalf
- Update CAQH periodically
- Monitor for Medicare revalidations and update applications as necessary
- Keep health provider qualifications file accurately compiled and frequently updated
IPMS provides payer contracting services to help practices find the revenue opportunities they’ve been missing. We have cultivated strong payer relationships for more than 20 years–and we leverage that insight alongside our expertise with every new client engagement. Our Account Managers work collaboratively with your practice to effectively alleviate the burden from your staff and maximize payer reimbursements.
- Identify areas of opportunity for increased rates and avoid leaving money on the table
- Bring consistency and organization to your payer contracts
- Save time and reduce operational costs and staff burden
- Reduce risk to your practice’s bottom line
- Assure that rate increases are applied timely and accurately
- Manage all aspects of payer contracts and negotiate on new relationships on your behalf
- Provide comprehensive reimbursement analysis
“IPMS is doing a great job for Advanced DermCare! From leadership (Liz and Melanie) to our account representative (Chris) to the billing team (Brenda and Shelley) – everyone at IPMS provides exceptional customer service. Plus, IPMS is proactive in managing claims and denials ensuring an efficient revenue cycle operation with minimal payment delays. I highly recommend IPMS as a billing partner!”
Advanced DermCare